The Lungs: Overview, Histology and Pathology
Respiration is a fundamental process to produce energy and sustain life. Oxidation of food and nutrition to produce energy require oxygen to form carbon dioxide and water. The respiratory system enables oxygen to enter in the body and carbon dioxide to leave it. The respiratory system has the function of conducting the air and permit the gas exchange between the body the external. The main function of the lung is filtrating the air and allowing the passage of oxygen and carbon dioxide to the cardiovascular system to be distributed to all tissues and eliminating the carbon dioxide produced by cells. The gas exchanges occur in the alveoli, which maximises surface area whilst minimising the barrier to diffusion from the airspace to the circulation [1].
Most of the respiratory epithelium is ciliary pseudostratified columnar epithelium, constituted by 5 type of cells: ciliated, goblet, basal, brush and neuroendocrine cells. Those cells collaborate to warm, moisturize and remove particles that enter in the system during the respiration. Alveolar epithelium is composed to type I pneumocytes, type II pneumocytes, and the occasional brush cell. Alveolar macrophages are also present in the alveolar walls.
The pathologies that affect the lung are classified into:
- Obstructive lung disease (emphysema, asthma, bronchiectasis and chronic bronchitis);
- Restrictive lung disease (acute and chronic forms, subdivided by etiology, characterized by fibrosis or alveolar septae);
- Infectious disease (typical or atypical community-acquired pneumonia; nosocomial pneumonia; aspiration; necrotizing pneumonia; chronic pneumonia; and pneumonia in immunocompromised hosts);
- Neoplastic disease (small cell lung carcinoma and non-small cell lung carcinoma).
Lung Biopsy – Preclinical Models
Lung biopsy can be performed in open (during surgery) or closed method (biopsy needle) to diagnose and monitor the progression of lung diseases, when abnormalities had been found on chest X-ray, CT scan or other imaging tests[2].
In vitro expansion of human airway epithelial cells can derivate from:
- endobronchial brushings [3];
- endobronchial biopsies or explants [4]
- Lung biopsies or lung explants digested to obtain a cell suspension[5]
- organoid derivation from cryo-preserved primary lung tumors[6]
- cadaveric organs via perfusion decellularization [7].
3D culture models recapitulating in vivo microarchitecture and physiology can be also grouped in: (i) organotypic explant cultures(including precision-cut lung slices); (ii) cellular spheroids; and (iii) tissue-engineered models [8]. Current protocols limit the number of sites capable of performing autologous airway cell therapies to those with both appropriate clinical and research facilities. Although standardized protocols for lung tissue engineering have been reported, the airway cells isolations, recellularization, and in vitroexpansion is just begging to grasp the complexity of the Lungs preclinical model [7].

Figure 1. Schematic representation of alternative methods to derive primary human airway epithelial cells from living donors by lung biopsy or brushing. Adapted image, CC by Gowers at al[9].
Lung Biopsy: evidence-based medicine and personalized medicine translated in novel in vitro technologies
Laboratory medicine and technologies for evidence-based medicine and personalized medicine are the cornerstones of innovation in medical field [10]. The unmet need of finding novel platform for diagnostic and therapeutic investigation is the main bottleneck in the pharmacology investigations.
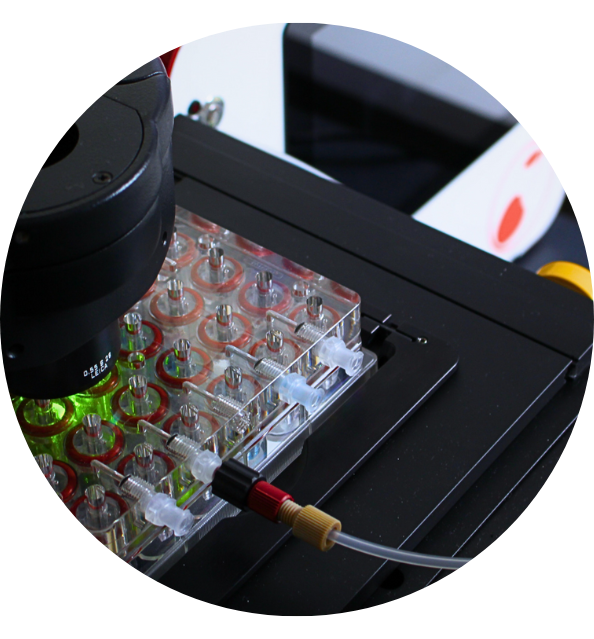
The lung has a unique mechanical environment and a unique cellular composition. Preclinical models as such cell and tissue cultures in static condition and laboratory animals represent the standard option in pharmacology investigation. However, the ethical sensitivity of citizen is pushing researchers on finding alternative closely to human physiology. Researchers are moving forward tissue-engineered organoids, cell culture and tissue explants (including lung biopsy) in (multi)organ-on-a-chip or 24 or 6 multi-wells plates in microfluidic devices[11]. In vitrolung modelling is a thriving and rapidly evolving field proving to change the drug discovery methodology, study cancer, and other diseases [8]. Beyond the recent advanced in translational research, novel tool for controlling the physiological condition are required to step forward in pathologies studies and drug development, by closely resembling of the lung’s microarchitecture.
References
[1] K. M. Akram et al., “Live imaging of alveologenesis in precision-cut lung slices reveals dynamic epithelial cell behaviour,” Nat. Commun., vol. 10, no. 1, 2019.
[2] M. M. Wahidi, F. J. F. Herth, and A. Ernst, “State of the art: Interventional pulmonology,” Chest, vol. 131, no. 1, pp. 261–274, 2007.
[3] S. G. Kelsen, I. A. Mardini, S. Zhou, J. L. Benovic, and N. C. Higgins, “A technique to harvest viable tracheobronchial epithelial cells from living human donors.,” Am. J. Respir. Cell Mol. Biol., vol. 7, no. 1, pp. 66–72, 1992.
[4] P. M. de Jong, M. A. J. A. van Sterkenburg, J. A. Kempenaar, J. H. Dijkman, and M. Ponec, “Serial culturing of human bronchial epithelial cells derived from biopsies,” Vitr. Cell. Dev. Biol. – Anim. J. Soc. Vitr. Biol., vol. 29, no. 5, pp. 379–387, 1993.
[5] F. Goulet et al., “Morphologic and Functional Properties of Bronchial Cells Isolated from Normal and Asthmatic Subjects,” Am. J. Respir. Cell Mol. Biol., vol. 15, no. 3, pp. 312–318, 1996.
[6] A. J. Walsh, R. S. Cook, M. E. Sanders, C. L. Arteaga, and M. C. Skala, “Drug response in organoids generated from frozen primary tumor tissues,” Sci. Rep., vol. 6, no. January, pp. 1–12, 2016.
[7] S. E. Gilpin and H. C. Ott, “Using nature’s platform to engineer bio-artificial lungs,” Ann. Am. Thorac. Soc., vol. 12, pp. S45–S49, 2015.
[8] D. Konar, M. Devarasetty, D. V. Yildiz, A. Atala, and S. V. Murphy, “Lung-On-A-Chip Technologies for Disease Modeling and Drug Development,” Biomed. Eng. Comput. Biol., vol. 7s1, p. BECB.S34252, 2016.
[9] K. H. C. Gowers, R. E. Hynds, R. M. Thakrar, B. Carroll, M. A. Birchall, and S. M. Janes, “Optimized isolation and expansion of human airway epithelial basal cells from endobronchial biopsy samples,” J. Tissue Eng. Regen. Med., vol. 12, no. 1, pp. e313–e317, 2018.
[10] R. S. Markin and S. A. Whalen, “Laboratory automation: Trajectory, technology, and tactics,” Clin. Chem., vol. 46, no. 5, pp. 764–771, 2000.
[11] N. Palechor-ceron et al., “Cancer Models and Next-Generation Living Biobanks,” 2019.

Discover the CubiX
Emulating human cell & tissue physiology