Breast Biopsies and Breast Cancer
Breast cancer is the most common female cancer worldwide with the highest rate of mortality for all cancers (15%). The incidence of breast cancer will affect 1-in-6 to 1-in-8 women (Fig. 1a) in their lifetime, impacting 2.1 million women per year, with 627 000 deaths reported for 2018 [1]. The incidence of breast cancer is increasing globally, with poor prognostic outcome and high mortality rates directly correlated to late stage diagnosis. Developing countries typically have a higher rate of breast cancer associated mortality (Fig. 1b), attributed to poor infrastructure as well as cultural stigma [2]. Early detection of breast cancer allows or a high success rate of treatment with a high 5-year survival rate [1, 2], directly correlated with the geographic economic development level (Fig. 1a, 1b). Mid-to-late stage breast cancer is prone to metastasize, particularly to bone tissue or the lymphatic system, complicating treatment with a poor prognostic outcome.
Detection of breast cancer can be facilitated by regular self-examinations and clinical examinations (e.g. ultrasound, MRI & mammograms). Unusual growths or lumps found in the breasts are mostly benign or cysts, where a biopsy – guided by ultrasound; MRI or X-ray – will be used for histological analysis. The ideal breast tissue biopsy should be a representative sample of suspected diseased tissues as well as healthy tissues. Biopsies can be classified in the following:
- Fine-needle aspiration biopsy – The least invasive method, where a quick determination can be made whether the detected breast abnormality is fluid filled or solid.
- Core-needle biopsy – This biopsy is more invasive and can be done with the assistance of ultrasound or MRI, where an incision will be made in the breast to allow for the core-needle to obtain a few tissue samples.
- Stereotactic biopsy – This procedure is done during a mammogram, where the radiologist will make a small incision in the breast and obtain tissue samples using a needle.
Technological advances have allowed for biopsy tissues to have a use beyond histology, where ex vivoculturing of breast tissue have allowed for advances in understanding breast cancer and associated metastases pathways. This increased knowledge base had advanced biomarker discovery [3], disease progression and metastasis [4], drug discovery [5] and drug response [6-9].
Ex vivo Culturing Methodologies for Breast Biopsy Derived Tissues
Breast cancer patient tissue derived models are being used more in research in recent literature, where it provides genetic and phenotypic relevancy compared to traditional 2D monoculture in vitromodels. Patient breast biopsy derived tissues can be used for research in various models (Fig. 2):
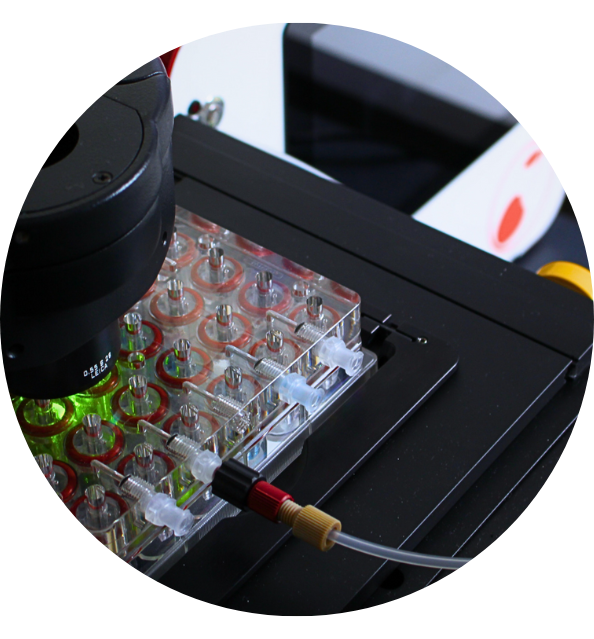
- Ex vivoculturing of tumour slices (e.g. precision cut) or processed biopsy tissues in static culture conditions [7], microfluidic systems [10] or perfused culturing bioreactor systems [9];
- Patient derived tumour cells for the 3D culturing or spheroids/organoids [10, 11]; and
- Patient derived xenografts (PDX) which use patient derived ex vivotissues for implantation on immunocompromised mice (e.g. athymic nude) [4, 11, 12].


Figure 1: The 5-year survival rate (a) for breast cancer as well as the (b) correlation of survival rate VS economic development level of various geographical regions. (Taken fromhttps://ourworldindata.org/).
Fabrication of patient derived 3D in vitrocancer models, whether from liquid biopsies or disaggregated cells, allow for a temporary genotype-phenotype relation. The use of spheroids and organoids generated in such a manner enables high-throughput drug response studies as well as the ability to create a biobank, however standardization of the technology, continuous culturing whilst maintaining phenotype/3D conformation and general static cell culture challenges (e.g. handling, contamination, etc.) remain. More complex 3D culturing approaches for creating in vitromodels; e.g. organ-on-chip, bioprinting and tissue engineering; provide better physiological recapitulation and maintenance of pathological phenotypes at the cost of increasing the complexity of required culturing homeostasis (e.g. temperature, oxygen gradients, nutrient penetration, etc.) in static culturing conditions. Cancer-associated molecular mechanisms, such as metastasis and drug resistance, is sensitive to hypoxia [13] and nutrient gradients [14], difficult to control in tissues where the dimensions are above 250µm in the absence of vasculature or advanced culturing systems. The time to culture cells for feasible use can take anywhere from 7 days to a few weeks, depending on the tissue type, where the media composition can influence the phenotype [7, 15].
Perfusion culturing provides synthetic vasculature by means of electromechanical pumps, temperature controllers and gas diffusion systems. These systems are however expensive and require significant financial investment, accessible only for well-funded institutions. Additionally, the variety of instruments on the market makes standardization difficult, leading to slow adoption in the greater research community.

Figure 2: Applications for patient biopsy derived breast tissues. The excised biopsy can be processed to various manageable slices for tissue culturing, xenografted onto immunodeficient mice or disaggregated for cell isolation. Isolated cells, cancerous and non-cancerous, can be used to generate various 3D in vitrotumour models or also be xenografted onto immunodeficient mice. The red arrows indicate the use of a biopsy tumour slice or excised xenografted patient derived tumours which can be used to generate various in vitromodels.
In vivoapproaches, such as xenografting, provides a physiological environment but the genetic relevancy between the implanted tissue and the host is not very high. Factors which should be considered during these types of models are: (i) physiological variance in absorption/distribution/metabolism/excretion; (ii) differential toxicology responses which do not always translate well into clinical trials; and (iii) no immunological responses. In addition to biological variation, it should be considered that these models are costly to establish, have a low grafting success rate (< 55%) with a long maturation timepoint (6 weeks to 6 months) and do not comply with the 3R (Replace-Reduce-Refine) approach.
Precision Oncology for Breast Cancer Using Tumour Slices
The disadvantage of patient biopsy derived in vitroand in vivomodels are the time required to deliver translatable results for the patient. Aggressive and metastatic cancers require immediate therapeutic intervention to provide the best prognostic outcome and the best 5-year survival rate post-therapy. Precision oncology requires a representative sample for the individual patient be utilized to find the best possible route of treatment based on unique genetic and phenotypic markers. Also, the ability to determine drug resistances and atypical toxicological effects for a class of compounds would facilitate clinicians to provide the best therapeutic strategy. The patient derived ex vivoculture would provide prolonged culturing to simulate continuous therapy such as with the patient.
Muraro et al [9] used breast cancer derived solid biopsy tissue with healthy and diseased tissues including the preserved cancer microenvironment, which was prepared into 2mm3 sections. The prepared biopsy samples were encapsulated between two porous collagen discs and perfused in a bioreactor for 14 days with phenotypes intact, compared to static culture which had a loss of phenotype within 72h. Drug response studies, using chemotherapy and immunotherapy, compared well with histology observed in patients. The system proved advantageous, however additional sample processing was required at predefined endpoints. Tumour cells and lymphocytes had high viable for most of the culturing duration.

Figure 3: The prolonged (14 days) culturing of ex vivotumour tissues (a). The application versatility of ex vivotumour tissue is schematically demonstrated in (b). (Image (a) is taken and adapted from [9] and (b) is taken and adapted from [7]).
Organotypic tumour slices (200-450µm) were cultured up to 7 days in static culture by Shivakumar et al [5], where the versatility of single-tissue origin ex vivoderived in vitromodels where demonstrated for drug discovery and toxicology. Grinshpun et al [16] used biopsy tissue from a patient with recurring metastasised breast cancer to determine the best therapeutic strategy by using next generation sequencing methods to find drug resistance biomarkers and accordingly planned their therapeutic strategy accordingly for an improved patient response – unfortunately the patient died suddenly during therapy. Grinshpun et al used 250µm tumour slices cultured in a rotating culture vessel, after using am intermediate rodent-based ex vivoculturing system. A tumour slice protocol used by Naipal et al [7] demonstrated successful culturing over 7 days of 150µm thick samples on a rotating shaker without loss of phenotype and included drug response studies. Naipal demonstrated that optimization of culture media was essential for increasing the viability time of the samples.
Ex vivo–in vitromodels of patient derived tissues have provided a novel method of rapid assessment of patient samples in a more direct manner, however there is currently no standardized and validated approach to allow for comparative analysis between research groups or clinicians. Additionally, ex vivopatient derived models struggle to recapitulate various culturing parameters (e.g. nutrient gradients, oxygen gradients, etc.) and do not readily allow for varying dose response and other pharmacodynamic assessment in a prolonged manner to fully recapitulate therapeutic duration for the patient. However, advances in technology and convergence of multidisciplinary approaches will slowly address these challenges to allow
References
- https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/
- Nyblade, H. et al. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Womens Health, 17:58.
- LaVallie, E.R. etal. Use of ex vivosystems for biomarker discovery. Current Opinion in Pharmacology, 8:647-653.
- Murayama, T. and Gotoh, N. Patient-Derived Xenograft Models of Breast Cancer and Their Application. Cells, 8:621
- Sivakumar, R. Organotypic tumor slice cultures provide a versatile platform for immune-oncology and drug discovery. ONCOIMMUNOLOGY, 8(12):e1670019.
- Carranza-Torres, I.E. et al. Organotypic Culture of Breast Tumour Explants as a Multicellular System for the Screening of Natural Compounds with Antineoplastic Potential. BioMed. Research Int., 618021
- Naipal, K.A.T., et al. Tumor Slice Culture System to Assess Drug Response of Primary Breast Cancer. BMC Cancer, 16:78.
- Van der Kuip, H. et al. Short Term Culture of Breast Cancer Tissues to Study the Activity of the Anticancer Drug Taxol in an Intact Tumor Microenvironment. BMC Cancer, 6:86.
- Muraro, M.G. et al. Ex-Vivo Assessment of Drug Response on Breast Cancer Primary Tissue with Preserved Microenvironments, ONCOIMMUNOLOGY, 6(7):e1331798.
- Aref, A.R. et al. 3D Microfludic Ex vivoCulture of Organotypic Tumor Spheroids to Model Immune Checkpoint Blockade.Lab Chip, 18:3129.
- DeRose, Y. S. et al. Patient-Derived Models of Human Breast Cancer: Protocols for In vitroand In vivoApplications in Tumor Biology and Translational Medicine. Current Protocols in Pharmacology, 14(23):1-43.
- Eckhardt, B.L. et al. Clinically Relevant Inflammatory Breast Cancer Patient-Derived Xenograft-Derived Ex vivoModel for Evaluation of Tumor-Specific Therapies, PLOSOne, 13(5):e0195932.
- Stone, J.K. et al. Hypoxia-Induced Cancer Cell-Specific Chromatin Interactions and Increases MALAT1 Expression in Breast Cancer Cells. J. Biol. Chem., doi:10.1074/jbc.RA118.006889
- Brodsky, A.N. et al. High Extracellular Lactate Causes Reductive Carboxylation in Breast Tissue Cell Lines Grown Under Normoxic Conditions. PLOSOne, 14(6):e0213419.
- Vu, B.T. et al. Optimization of Culture Medium for the Isolation and Propagation of Human Breast Cancer Cells from Primary Tumour Biopsies. Biomedical Research and Therapy, 2(2):207-219.
- Grinshpun, A. et al. Ex Vivo Organ Culture as Potential Prioritization Tool for Breast Cancer Targeted Therapy. Cancer Biology & Therapy, 19(8):645-648.

Discover the CubiX
Emulating human cell & tissue physiology