Introduction
Organoid and artificial intelligence approaches are central to the FDA’s roadmap for reducing animal use in preclinical safety studies. The Agency highlights new approach methodologies (NAMs) such as microphysiological systems (MPS such as organoids and organ‑on‑chips), advanced in vitro assays, and in silico modeling, aligned with the FDA Modernization Act 3.0 to formalize qualification of nonclinical methods. Together, these initiatives aim to generate human‑relevant, mechanism‑based evidence for INDs and research.
Delivering on this vision requires bioconvergence, that is, coordinated advances across biology, engineering, computational science, and AI. In practice, model‑informed, AI‑based in silico predictions may guide experiments for validation in MPS. High‑content assays (live imaging and multi‑omics) then capture comprehensive cell states so that, finally, machine learning integrates heterogeneous data to refine models, de‑risk first‑in‑human decisions, and improve translatability.
In the sections that follow, we examine how breast cancer organoids and breast‑ cancer‑on‑chip systems combined with imaging and omics, enable actionable insights for disease modeling, personalized medicine, and drug screening, thus highlighting practical intersections of breast cancer organoid and AI / machine learning for high‑content screening and decision support.
Learn more about our ready to use breast cancer organoid models.
New technologies in the era of personalized medicine: Organoids, AI and OMICs in breast cancer
A major driver of precision oncology today is the convergence of organoid and artificial intelligence methods with high‑content omics readouts. While this convergence is emerging now, each of these models and assays have been used independently in the breast cancer medical and research fields.
On the clinical front, AI for imaging is already transforming the field of breast cancer diagnosis: deep‑learning models for mammography, MRI, and digital pathology support risk stratification, detection, and prognosis by extracting patterns beyond human perception and standardizing reads across sites and devices. Machine learning–driven image analysis is also gaining traction in preclinical research, particularly in prognostic applications using patient-derived organoids (PDOs). These models, cultured directly from patient tumors, allow for parallel testing of multiple drug regimens. High-content imaging captures morphological responses, which can be rapidly processed and interpreted using AI to identify phenotype-treatment relationships and predict likely therapeutic outcomes. Alternatively, breast cancer organoid and AI strategies may apply similar imaging analysis techniques at the preclinical level with high‑content phenotyping of in vitro models for drug screening and disease modelling(1).
In parallel, multi‑omics have transformed personalized care. Genomics, transcriptomics, proteomics, and metabolomics provide molecular portraits that enable early detection, prognosis, therapy selection, and resistance monitoring, especially when integrated with network‑level analyses. These strategies reframe breast cancer from a single disease to molecularly defined entities(2).
Notably, a transformative milestone emerged with single‑cell sequencing. Since the first single‑cell RNA‑seq demonstration in 2009(3), single‑cell approaches have become central to mapping intratumoral heterogeneity. They resolve clonal diversity, malignant cell states, and stromal/immune components of the tumor microenvironment (TME) that shape progression and therapy response: insights highlighted by recent atlases and increasingly used to track resistance trajectories(4).
Finally, new approach methodologies (NAMs) such as microphysiological systems (MPS) (e.g. organoids, organ-on-chip) have opened practical routes to personalization. Notably, breast cancer organoids retain histopathology and key subtype markers (ER, PR, HER2), mirror genomic features of the original tumors, and enable high‑throughput drug screening and biobanking, making them credible ex vivo twins for rapid therapy testing and research‑grade repositories(5). These assets create a natural interface for breast cancer organoid and machine learning pipelines that couple imaging phenotypes with multi‑omics readouts.
Together, these technologies position breast cancer organoid and omics platforms, powered by AI, to deliver human‑relevant evidence at scale, linking mechanism to phenotype and, ultimately, to individualized treatment decisions.
Organoid and artificial intelligence: an integrated approach
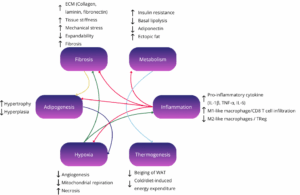
Organoid and artificial intelligence approaches are increasingly integrated, from model design to data analysis and translational decision‑making as reviewed by Bai et al, and Shi et al. In microphysiological systems (MPS), machine learning and optimization algorithms have the potential to accelerate the design and construction of organoids by identifying ideal culture conditions. For instance it may help tuning ECM architecture/composition (stiffness, viscoelasticity, ligand density…), geometry parameters for bioprinting, and culture media/growth‑factor cocktails (especially for iPSC differentiation) to achieve target phenotypes such as proliferation–differentiation balance, polarity, vascularization, or immunity. Compared with trial‑and‑error protocols, AI‑guided design may considerably reduce iteration cycles and improves reproducibility.
On the measurement side, AI is already applied for high‑content imaging and omics analysis. For imaging, state‑of‑the‑art computer vision quantifies multiscale phenotypes: morphology classes, budding and lumen formation, single‑cell trajectories, and treatment‑response dynamics in time‑lapse data. These labeling-free methods reduce handwork burden while enabling robust, quantitative phenomics. For multi‑omics (genomics, transcriptomics, proteomics, metabolomics, and single‑cell readouts), ML supports quality control, batch correction, feature selection, and network/pathway inference. AI already plays a key role in simplifying and accelerating the analysis of high-content screening data. The next critical step is to integrate imaging and omics into unified, mechanistically-informed models that not only capture complex biological responses but are also human-relevant. These integrated frameworks have the potential to become predictive enough to reduce or even replace the need for validation in traditional in vivo models.
In disease modelling and drug screening, AI workflows used on organoid and other in vitro models can predict efficacy and emergent resistance by linking image‑derived phenotypes to molecular programs, prioritize combinations via drug synergy modeling and reveal toxicity using multi‑tissue MPS (e.g., liver–heart) coupled to predictive models. As biobanks grow, organoid and machine learning frameworks can connect patient features to ex vivo responses and serve to guide decision making in personalized therapy(6,7).
Breast cancer organoid, AI and high-content analysis
Although organoid and artificial intelligence methods are rapidly expanding across oncology, reports that apply AI directly to high‑content imaging and –omics generated from in vitro breast‑cancer models remain relatively few. Two complementary patterns are emerging.
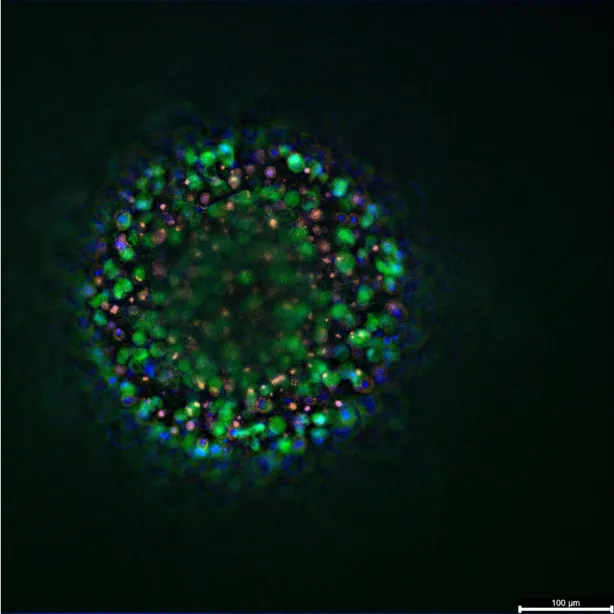
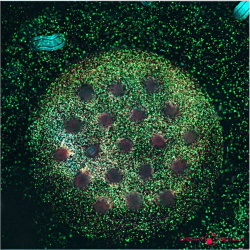
1 – AI to analyze organoid-derived -omics data: By using machine‑learning to structure large imaging datasets from breast‑cancer organoids or organoid‑like co‑cultures. For example, droplet‑microfluidic platforms have combined unsupervised clustering and simple supervised classifiers to segment ER‑positive organoids into proliferation states (via Ki67 intensity and size) and to quantify how adipose‑derived stem cells from different donors modulate endocrine response. This approach reveals microenvironment‑ and donor‑specific effects on endocrine resistance that bulk averages can obscure(8).
2 – AI for multi‑omics subtyping based on human database followed by functional validation in patient‑derived organoids (PDOs): For instance in triple‑negative breast cancer, metabolomic atlases integrated with genomics/transcriptomics have used computational models to define riskful subgroups and identify metabolic vulnerabilities (e.g., sphingosine‑1‑phosphate signaling in luminal androgen receptor tumors) that were subsequently confirmed in PDOs(9).
In the domain of disease modelling, Cherry Biotech participates in PLAST_CELL, a program supported by the European Innovation Council (EIC) designed to quantify cellular plasticity at the single‑cell level and link it to metastasis, therapy resistance, and aggressiveness. The platform integrates biomimetic 3D microenvironments built on our CubiX systems, high‑resolution live‑cell imaging, and machine‑learning analytics to deliver real‑time, single‑cell assessments of adaptation. The goal is a mechanistic plasticity score capable of predicting tumor behavior and informing clinical decision‑making. Learn more on our project pages: Cherry Biotech overview and CORDIS.
Looking forward, breast cancer organoid and AI workflows will increasingly link imaging‑defined phenotypes with single‑cell and bulk -omics to build human‑relevant predictors of efficacy, resistance, and toxicity. High‑content screening is evolving from descriptive readouts to mechanistic models powerful enough to prioritize therapies, guide personalized medicine, and ultimately reduce dependence on animal validation.
Resources
- Swanson K, Wu E, Zhang A, Alizadeh AA, Zou J. From patterns to patients: Advances in clinical machine learning for cancer diagnosis, prognosis, and treatment. Cell. avr 2023;186(8):1772‑91.
- Rossi C, Cicalini I, Cufaro MC, Consalvo A, Upadhyaya P, Sala G, et al. Breast cancer in the era of integrating “Omics” approaches. Oncogenesis. 14 avr 2022;11(1):17.
- Tang F, Barbacioru C, Wang Y, Nordman E, Lee C, Xu N, et al. mRNA-Seq whole-transcriptome analysis of a single cell. Nat Methods. mai 2009;6(5):377‑82.
- Tirosh I, Suva ML. Cancer cell states: Lessons from ten years of single-cell RNA-sequencing of human tumors. Cancer Cell. 9 sept 2024;42(9):1497‑506.
- Sachs N, De Ligt J, Kopper O, Gogola E, Bounova G, Weeber F, et al. A Living Biobank of Breast Cancer Organoids Captures Disease Heterogeneity. Cell. janv 2018;172(1‑2):373-386.e10.
- Bai L, Wu Y, Li G, Zhang W, Zhang H, Su J. AI-enabled organoids: Construction, analysis, and application. Bioact Mater. janv 2024;31:525‑48.
- Shi H, Kowalczewski A, Vu D, Liu X, Salekin A, Yang H, et al. Organoid intelligence: Integration of organoid technology and artificial intelligence in the new era of in vitro models. Med Nov Technol Devices. mars 2024;21:100276.
- Ortega Quesada BA, Chauvin C, Martin E, Melvin A. Droplet microfluidics integrated with machine learning reveals how adipose-derived stem cells modulate endocrine response and tumor heterogeneity in ER+ breast cancer. Lab Chip. 2025;25(15):3817‑30.
- Xiao Y, Ma D, Yang YS, Yang F, Ding JH, Gong Y, et al. Comprehensive metabolomics expands precision medicine for triple-negative breast cancer. Cell Res. 1 févr 2022;32(5):477‑90.
FAQ
The FDA has a roadmap to reduce animal use. It highlights new approach methodologies (NAMs). These include microphysiological systems (MPS), like organoids, and computational (in silico) modeling. The FDA Modernization Act 3.0 supports formalizing the qualification of these nonclinical methods. This initiative aims to generate human-relevant, mechanism-based evidence for research and new drug applications (INDs). This requires bioconvergence, which coordinates biology, engineering, and computational science. Computational predictions may guide experiments, which are then confirmed in MPS.
A convergence of organoid methods and computational analysis, along with high-content omics, is a main force in precision oncology. Computational analysis is already used in clinical imaging for diagnosis and prognosis. In preclinical research, automated image analysis is used with patient-derived organoids (PDOs). PDOs are cultured from patient tumours and permit parallel drug testing. High-content imaging captures morphological responses. Automated methods are then used to process these images. These methods can identify relationships between phenotype and treatment. This helps predict therapeutic outcomes.
Patient-derived organoids, or PDOs, are cultured directly from patient tumours. They are considered new approach methodologies, or NAMs. These models have been shown to retain the histopathology of the original tumour. They also retain important subtype markers, such as ER, PR, and HER2. The genomic features of the original tumours are also mirrored in the PDOs. They are used for high-throughput drug screening. Biobanking of these models is also possible. Because they are sourced from patients, they are seen as credible ex vivo twins for rapid therapy testing.
Organoid and computational analysis methods are increasingly integrated. Algorithmic methods have the capability to speed up the design and construction of organoids. This is done by identifying ideal culture conditions. For instance, computational analysis may help tune the ECM architecture, such as its stiffness or ligand density. It can also help define geometry parameters for bioprinting. The selection of culture media and growth-factor cocktails may also be guided by these methods. This is especially true for iPSC differentiation. When compared with traditional trial-and-error protocols, this guided design may greatly reduce iteration cycles. It may also improve reproducibility.
Automated analysis is applied to high-content imaging and omics analysis. For imaging, state-of-the-art computer vision is used. It quantifies multiscale phenotypes. This includes morphology classes, budding, and lumen formation. Single-cell trajectories and treatment-response dynamics in time-lapse data are also quantified. These methods reduce the handwork burden. They also permit quantitative phenomics. For multi-omics readouts, algorithmic methods support quality control, batch correction, and feature selection. Network and pathway inference is also supported. This process plays a central part in simplifying the analysis of high-content screening data.
Bioconvergence is the coordinated advance across biology, engineering, computational science, and automated analysis. It is needed to deliver on the vision of replacing animal studies with new methods. In practice, model-informed, computational predictions may be used. These predictions guide experiments that are then confirmed in microphysiological systems (MPS). High-content assays, such as live imaging and multi-omics, are used to capture comprehensive cell states. Finally, algorithmic methods integrate this heterogeneous data. This integration is used to refine models. It also helps to de-risk first-in-human decisions. Translatability of research may be improved by this process.
Multi-omics have altered personalized care. Genomics, transcriptomics, proteomics, and metabolomics are used. These methods give molecular portraits of a tumour. These portraits allow for early detection and prognosis. Therapy selection and resistance monitoring are also supported by this information. This is especially true when the data is integrated with network-level analyses. These strategies reframe breast cancer. It is viewed as a collection of molecularly defined entities rather than a single disease. This detailed information is used to make individualized treatment decisions.
Single-cell sequencing has become central to breast cancer research since its first demonstration. Its main application is mapping intratumoral heterogeneity. This means it can resolve the clonal diversity within a single tumour. Different malignant cell states can be identified. The components of the tumour microenvironment (TME) are also resolved. These components include stromal and immune cells. These TME components are known to shape tumour progression. They also shape the response to therapy. These findings are highlighted by recent atlases. The methods are increasingly used to track resistance trajectories in patients.
One pattern involves using computational methods to structure large datasets from breast-cancer organoids. For example, droplet-microfluidic platforms were used. These combined unsupervised clustering with simple supervised classifiers. This was done to segment ER-positive organoids into different proliferation states. This segmentation was based on Ki67 intensity and size. The method also quantified how adipose-derived stem cells from different donors modulated the endocrine response. This approach showed microenvironment- and donor-specific effects on endocrine resistance. These are details that bulk averages can obscure.
A second pattern involves using computational models for multi-omics subtyping. This subtyping is based on human databases. Functional confirmation of the findings is then performed using patient-derived organoids (PDOs). An example was seen in triple-negative breast cancer. Metabolomic atlases were integrated with genomics and transcriptomics. Computational models defined riskful subgroups from this data. Metabolic vulnerabilities were also identified. One such vulnerability was related to sphingosine-1-phosphate signaling in luminal androgen receptor tumours. This finding was subsequently confirmed in PDOs.