Introduction
Melanoma is clearly a complex disease with a high degree of heterogeneity and adaptability. Melanoma cells are part of a larger ecosystem in which the tumor microenvironment influences their evolution and ability to evade medication therapy. In order to acquire a better knowledge of the mechanisms behind melanoma biology and therapeutic resistance, various efforts have lately been directed toward the development of ex-vivo models capable of replicating the living conditions of melanoma cells in real patients.
The researcher has created and applied a novel approach that uses complex 3D models in microfluidic systems to replicate the melanoma immune microenvironment.
How to culture vascularized & immunocompetent 3D models in a standard Multiwell
Abstract
The authors state that “Malignant melanoma still remains a cancer with very poor survival rates, although it is at the forefront of personalized medicine. Most patients show partial responses and disease progressed due to adaptative resistance mechanisms, preventing long-lasting clinical benefits to the current treatments.
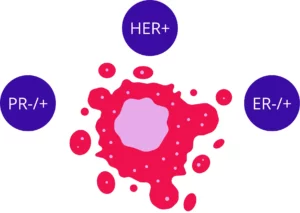
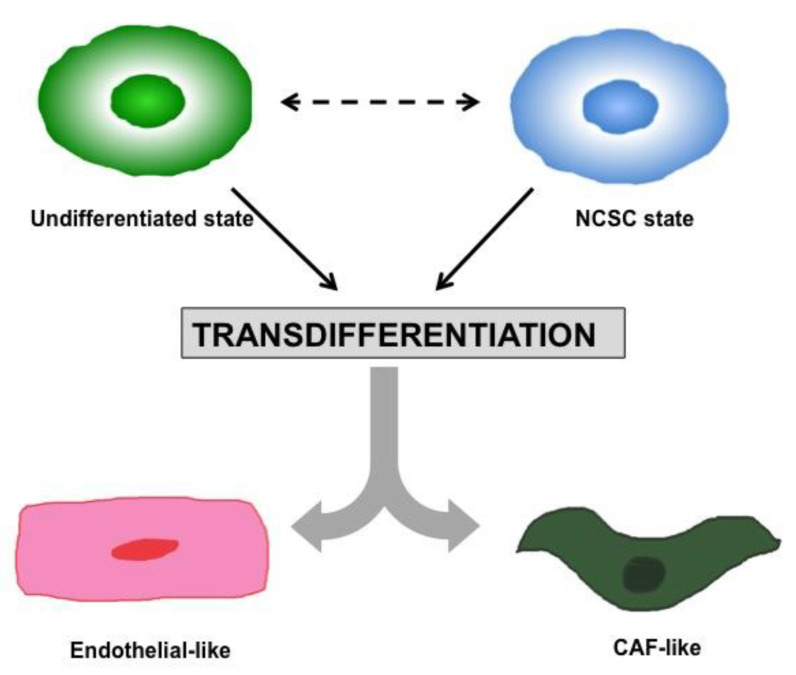
The response to therapies can be shaped by not only taking into account cancer cell heterogeneity and plasticity but also by its structural context as well as the cellular component of the tumor microenvironment (TME).
Here, we review the recent development in the field of immunotherapy and target-based therapy and how, in the era of tumor micro-tissue engineering, ex-vivo assays could help to enhance our melanoma biology knowledge in its complexity, translating it into the development of successful therapeutic strategies, as well as in the prediction of therapeutic benefits.”.
References
Varrone F, Mandrich L, Caputo E. Melanoma Immunotherapy and Precision Medicine in the Era of Tumor Micro-Tissue Engineering: Where Are We Now and Where Are We Going? Cancers (Basel). 2021 Nov 18;13(22):5788. doi: 10.3390/cancers13225788. PMID: 34830940; PMCID: PMC8616100.
FAQ
Melanoma is described as an intricate disease. It shows a high degree of variation and a strong ability to change. Malignant melanoma is associated with low survival rates, even though it is at the leading edge of personalised medicine. Melanoma cells exist within a larger system. This system is the tumour microenvironment (TME). The TME has an effect on the evolution of the cells. It also affects their capacity to evade medication therapy. A majority of patients show only partial responses to current treatments. The disease often advances. This progression is caused by adaptive resistance processes. These processes stop sustained clinical benefits from being achieved. This resistance and variation make the disease difficult to manage effectively.
The response to melanoma therapies is determined by several factors. It is not only formed by cancer cell variation and plasticity. The structural context of the tumour is also a consideration. Furthermore, the cellular parts of the tumour microenvironment (TME) play a part. To understand why treatments fail, these elements are studied. The TME is the larger system in which the melanoma cells exist. Its cellular parts can affect how the cancer evolves and resists medication. By examining the cancer cells, their structure, and their environment together, a better understanding can be gained. This is necessary because many patients only have partial responses to treatments.
Recent efforts have been directed toward the creation of ex-vivo models. The purpose of these models is to copy the living conditions of melanoma cells as they are found in patients. These models are being developed to gain a better understanding of the processes behind melanoma biology. They are also intended to provide insight into therapeutic resistance. Current treatments often result in only partial responses. Resistance processes develop that prevent sustained benefits. Ex-vivo assays, as part of tumour micro-tissue engineering, could help increase the understanding of melanoma’s intricate nature. This improved understanding might then be applied to the creation of effective therapeutic plans. These models may also assist in forecasting therapeutic benefits for patients.
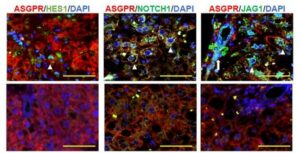
A new method has been created and applied by researchers. This method is used to study the melanoma immune microenvironment. It involves the use of intricate 3D models. These models are contained within microfluidic systems. The goal of this application is to recreate the specific conditions of the immune microenvironment found in melanoma. This allows for a more detailed study of the tumour and its surroundings outside of a patient. This approach is part of a wider effort to build better ex-vivo models. Such models are needed to understand why melanoma is able to evade medication and how its biology functions. The insights from these 3D systems could help in forming new treatment plans.